Basal Thumb Joint Replacement
The Importance of the Basal Thumb Joint
Indispensable Functions of the Hand
The hand’s intricate anatomical structures enable people to complete all kinds of complicated tasks from playing a piano to operating complex machines. The hand allows people to grip tools, carry objects, and hold on to one another.
The thumb’s contribution to hand function is close to 40%. Therefore, any pain, disability, or loss of function of the thumb poses significant challenges in terms of quality of life and activities of daily living.
The Basal Thumb Joint is Known as the First Carpometacarpal Joint (CMCJ)
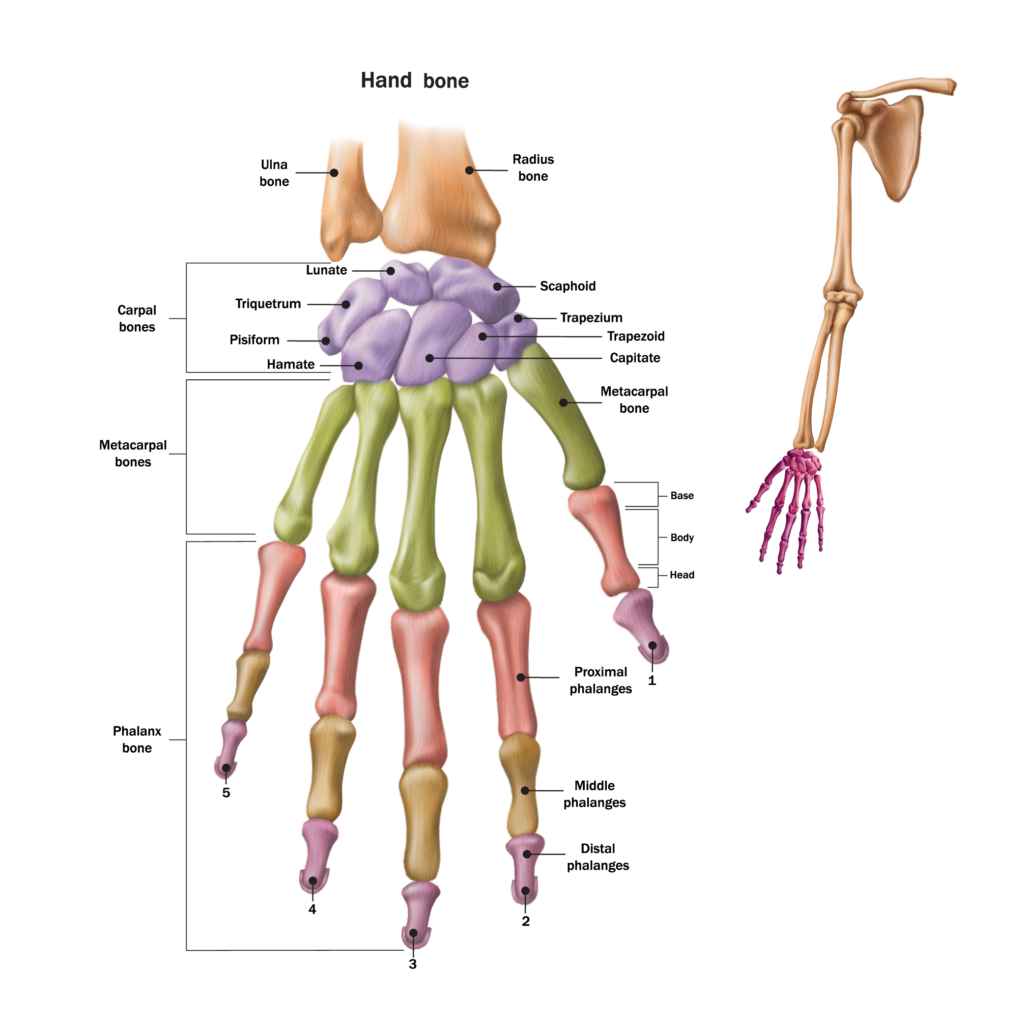
The articulation of the thumb is possible due to the complex and ingenious design of the saddle-shaped joint consisting of carpal and metacarpal bones at the base of the thumb. Muscles and ligaments provide strength and stability which allow the thumb to move. The first CMCJ is surrounded by a capsule which creates additional stability while providing lubricating synovial fluid for the joints. Cartilage between the joints provides cushioning which makes thumb movements smooth and comfortable.
Arthritis of the Basal Thumb Joint or First CMCJ

Hand Arthritis
The two types of hand arthritis are inflammatory arthritis such as rheumatoid, gout, or psoriatic arthritis and degenerative arthritis, which is also known as osteoarthritis. Most commonly, basal thumb arthritis is osteoarthritis. This is the wearing down of the cushioning cartilage between the joints.
What Causes Basal Thumb Osteoarthritis and What Are the Symptoms?
Basal thumb osteoarthritis is the result of premature wearing down of the cartilage surfaces in a joint. Chronic overuse of the basal thumb joint or excessive use involving forceful pinching may cause unnecessary wear and tear. This may also be the result of age-related degeneration. An injury or joint damage as well as developmental deformities are other causes of early wearing down of cartilage.
Basal thumb arthritis symptoms typically include discomfort and pain at the base of the thumb when gripping or pinching an item. There may be decreased range of movement and reduced strength with pinching and gripping as well. These symptoms are commonly associated with stiffness, swelling, tenderness, and an aching sensation after prolonged use of the thumb. Symptoms tend to worsen over time. The joint may become enlarged or there may be prominent bones or lumps.

Diagnosis, Risk Factors, and Non-operative Treatment
CMCJ Osteoarthritis Diagnosis
Diagnosing first CMCJ osteoarthritis is performed in a clinical setting with a doctor. A general doctor may refer the patient to a Hand Specialist. The Hand Specialist will examine the symptomatic hand. A diagnosis of basal thumb arthritis may be determined with a detailed patient history along with physical examination of the hand. It is important to differentiate basal thumb osteoarthritis from other types of arthritis as well as other potential wrist, hand, and thumb issues. First CMCJ osteoarthritis is often associated with other conditions of the hand and wrist including carpal tunnel syndrome, trigger digits, tenosynovitis, MCP hyperextension, and scaphotrapezial arthrosis. To confirm the diagnosis and develop a treatment plan, a Hand Specialist may perform x-rays, nerve conduction studies, blood tests, and joint fluid analysis.
Risk Factors of first CMCJ Osteoarthritis
- Previous injury of the joint or occupational hazards that require overuse of the thumb.
- Wearing down of cartilage is a normal part of the aging process, therefore, age-related joint degeneration is a risk factor for people over the age of 40.
- first CMCJ osteoarthritis is more common in female patients.
- Lifestyle factors such as activity level, diet, and obesity may affect the risk of first CMCJ osteoarthritis.
- Genetic predisposition to joint issues may also increase risk of first CMCJ osteoarthritis.
Non-operative Treatment Options for first CMCJ Osteoarthritis
Treating osteoarthritis of the base of the thumb is similar to treating osteoarthritis in other joints of the body. The goal of non-operative treatments is to minimize stress on the joint to thus reduce progressive degeneration of the joint. Non-operative treatments also aim to manage pain and inflammation of the effected joint.
Non-surgical treatments may include:

- Limit range of motion by using custom or over the counter rigid splints or braces.
- Modify activities to reduce stress on the joint.
- Medication for pain relief.
- Stretching and range-of-motion exercises to improve joint stability, strength, and thumb motion.
- Joint support which may include lifestyle and diet changes as well as joint supporting supplements such as glucosamine and calcium.
- Injections to the joints with may include corticosteroids for pain or viscoelastic formulations to assist the joint to continue moving smoothly and comfortably.

Surgical Treatment Options
When is Surgery Recommended?
As osteoarthritic conditions tend to worsen over time, the effectiveness of non-surgical treatments may diminish. After all non-surgical solutions have been exhausted and the patient continues to suffer discomfort, pain, or decreased function of the thumb, it is time to consider surgical intervention.
Types of Surgical Care
Arthroscopic Debridement
Arthroscopic debridement is a minimally invasive procedure where a small telescope is inserted into the joint through tiny keyhole incisions. The joint is cleaned up, removing any loose material, extra bone, and inflammation which has developed and causes stiffness and pain.
Joint Balancing and Fusion
Joint balancing and fusion procedures include cutting bone and changing joint angles. The bones are fixed in place with metal implants. This allows the bones to grow or fuse together. There is loss of mobility which aims to eliminate associated pain. Pinch and grip strength is preserved.
Arthroplasty – Three Types
Arthroplasty procedures involve joint moulding, ligament reconstruction, and tendon interposition as well as joint replacement surgery. There are three types:
Excisional arthroplasty is the removal of the affected joint. The procedure may include bone stabilization.
Interpositional arthroplasty uses joint cushioning techniques by using tendon grafts made of the patient’s tissue. This provides relief of inflammation because it cushions the worn-out cartilage.
Replacement arthroplasty surgery is the removal of the normal joint which is replaced by an artificial joint implant.
The type of operation chosen is specific to each patient and their degree of degenerative change. Each type of surgery has pros and cons relative to the stage of arthritis and the predicted functionality of the joint post-surgery.
Recovery depends on several factors and may take between 8 weeks to a year. Ongoing therapy provided by occupational or physical therapists may increase the positive outcomes after surgical intervention.
Possible Complications of First CMCJ Surgery
Any surgical procedure is not without risks. Basal thumb surgery is no exception. Possible surgical complications are infection, bleeding, and/or nerve or tendon damage.
Specific potential complications associated with surgical intervention for first CMCJ osteoarthritis are:
Arthroscopic procedures carry a risk of developing septic arthritis or inadvertent cartilage damage.
Joint balancing and fusion procedures carry a risk of non-union or malunion resulting in inflammation of surrounding tissue and pain.
Excisional and interpositional arthroplasty procedures carry a risk of instability and pain recurrence.
Replacement arthroplasty risks are dislocation or loosening of the implant as well as premature wear of the artificial joint’s components.
Advantages of the TOUCH® CMCJ Dual-Mobility Prosthesis
When joint replacement arthroplasty is deemed to have high potential for a positive outcome for basal thumb arthritis, there are many choices of artificial joints available.
TOUCH® CMCJ Dual-Mobility Prosthesis is a new type of artificial joint that allows for more articulation of the joint. It is designed with 144 customizable options to fit each patient’s unique anatomy.
The advantages of total joint replacement with TOUCH® CMCJ Dual-Mobility Prosthesis have shown reduced postoperative pain, faster functional recovery, and improved pinch and grip strength.
CHARMS is the first organisation in Singapore and Asia to be certified to use TOUCH implants in treatment of CMCJ arthritis.
Results and Case Study at CHARMS
Evaluation of 23 patients who received TOUCH® CMCJ Dual-Mobility Prosthesis between September 2018 and July 2020 at CHARMS.
The patients ranged in age from 43 to 67. The study included 12 male patients and 11 female patients.
Postsurgical therapy included:
- Wearing a custom long thumb spica orthosis intermittently for 3 weeks.
- Pain and swelling were controlled for the first two weeks post-surgery.
- Hand therapy during the first two weeks post-surgery included range-of-motion exercises.
- At four weeks post-operatively, strengthening exercises were initiated and therapy progressed according to each patient’s needs.
Mean Overall Improvement of 23 Patients Post CMCJ Replacement with TOUCH® CMCJ Dual-Mobility Prosthesis*
| PREOPERATIVELY | POSTOPERATIVELY | |
| Quick DASH* | 41 = SEVERE DIFFICULTY | 11 = GOOD FUNCTIONAL OUTCOME |
| PINCH AND GRIP STRENGTH | Pinch strength = 6 kgf Grip strength = 24.9 kgf | Pinch strength = 5.6 kgf. Up 93% at 4 weeks post-op. Grip strength = 20.9 kgf. Up 83% at 4 weeks postoperatively. |
| RANGE OF MOTION | Full range-of-motion was regained at 24 days postoperatively, on average. | |
| PAIN | Patients attained a pain-free thumb 31 days postoperatively, on average. | |
| (VAS)* VALUES FOR PAIN | 7/10 | 4/10 |
*Disabilities of the Arm, Shoulder and Hand (QuickDASH) score outcomes.
*Visual analogue scale (VAS) values for pain.
The study at CHARMS assessing the TOUCH® prosthesis shows a significant improvement in QuickDASH scores, pain reduction, improved range of motion, and pinch and grip strength.
How CHARMS Can Help Symptoms and Pain of CMCJ Arthritis
The hand’s intricate structure includes an incredible articulating thumb which contributes to 40% of the hand’s function. It is important to see a doctor if there is pain, discomfort, or limited function of the thumb, hand, or wrist. At CHARMS, the highly specialised Hand Surgeons guide a dedicated team of Hand Occupational Therapists, Hand Physiotherapists, Splint Fabrication Specialists, and Nurses who make every effort to provide the highest level of service and care. The hand care team at CHARMS has extensive knowledge and microsurgical expertise to provide treatment for conditions associated with arthritis of the basal thumb.
The CHARMS hand care team is dedicated to easing your hand pain, discomfort, and limited function so you can get back to enjoying all your hands do for you. Speak to the caring hand specialists at CHARMS at +65 6733 9093. Or book an appointment for a consultation, diagnosis, and treatment plan options.
Can we help you?
